Objective To evaluate the efficacy and prognosis of percutaneous vertebroplasty/ kyphoplasty (PVP/PKP) in patients with newly diagnosed multiple myeloma (NDMM).
Methods Clinical data of NDMM patients who underwent PVP/PKP during front-line regimen at Peking Union Medical College Hospital from January 1 2003 to June 30, 2023, were retrospectively analyzed. Patients with comparable severity of bone disease and no orthopedic surgery were selected as controls. Visual analogue scale (VAS) score, progression-free survival (PFS), and overall survival (OS) were compared. Statistical methods mainly adopt χ 2-test, t-test, Kaplan Meier, and COX regression analysis.
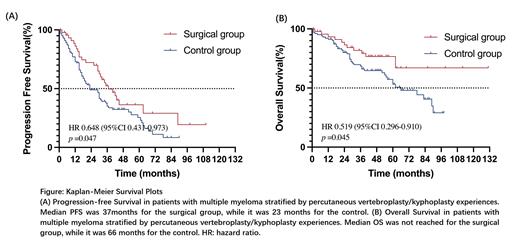
Results Baseline characteristics were matched between the surgical group (n=51 with 56 surgeries) and non-surgical group(n=102), including gender, age, paraprotein type, serum M protein level, International Staging System(ISS), numbers of lytic lesions, cytogenetic abnormalities, first-line treatment, and autologous stem-cell transplantation (ASCT)( P>0.05). Bone lesions for PVP/PKP were located at thoracic vertebrae (53.6%, 30/56) or lumbosacral vertebrae (46.4%, 26/56). The postoperative VAS score was significantly improved (2.25±0.81 vs 5.92±1.05 , P<0.001). The median follow-up time was 51[38,70] months. Kaplan-Meier survival analysis suggested that PFS (37[17,89] vs 23[12.61] months, HR 0.648, 95%CI 0.431-0.973, P=0.047) and OS (not reached vs 66[28, NR] months, HR 0.519, 95%CI 0.296-0.910, P=0.045) in the surgical group were significantly improved. COX multivariate analysis suggested that PVP/PKP was an independent prognostic factor for PFS ( P=0.021, HR 0.589,95%CI 0.376-0.922)and OS( P=0.038, HR 0.496,95%CI 0.255-0.963), while not receiving ASCT or ISS stage II/III were independent risk factors. Subgroup analysis confirmed that patients with ISS II/III or non-ASCT achieved better PFS and OS in the surgical group(PFS: P=0.033, P=0.040; OS: P=0.024, P=0.018), while patients with ISS I or receiving ASCT had similar survival outcome(PFS P>0.05; OS P>0.05) between two groups.
Conclusion For NDMM patients, PVP/PKP is associated better quality of life due to alleviating bone pain. Meanwhile, it improves the PFS and OS of patients with ISS stage II/III or non-transplant eligible, which suggests that shortening the gap from symptom onset to diagnosis by surgical pathology will improve response in MM.
Disclosures
No relevant conflicts of interest to declare.